The SARS-CoV-2 (COVID-19) pandemic has created an unprecedented demand for germicidal ultraviolet (UV) light irradiation equipment, marking a turning point for an underutilized technology for infectious disease control in buildings.
For nearly a century, ultraviolet germicidal technology has been effectively used to destroy surface and airborne microbes such as tuberculosis, measles, and more. But for reasons that are difficult to pinpoint, its applications have mostly been limited to such high-risk locations as emergency rooms and surgical suites. That changed in the months following the COVID-19 outbreak. Suddenly a variety of facilities from churches to hair salons were looking for ways to safely return to normal. Not surprisingly, their search led many to ultraviolet germicidal irradiation (UVGI), and specifically to upper-room (UVGI), as a way to mitigate the risk of infection. This paper will explain in a manner that is accessible to all building owners and managers what upper-room UVGI is, how upper-room UVGI differs from other UV strategies, and what makes it a particularly relevant solution for a wide range of mainstream applications today.
For those that may be unaware, it should be emphasized that UVGI is neither new nor unproven. Its effectiveness at microbial inactivation has been studied and well-documented since the 1930s. It has been successfully used to control the spread of pocketed outbreaks of measles and tuberculosis and it also has been used to destroy additional air and surface microbes including chickenpox, mumps, and cold viruses. Furthermore, the Center for Disease Control (CDC) and the American Society of Heating, Refrigerating and Air-Conditioning Engineers (ASHRAE) have all recognized UVGI as effective at controlling the spread of viral and bacterial microbes.
All this being the case, why hasn’t germicidal ultraviolet (UV-C) light been applied with greater regularity in buildings? And why haven’t we heard more about the technology?
There is no single answer except perhaps to say that historically pharmacology and vaccines have taken center stage when it comes to eradicating infectious diseases. As a society, we have transitioned over time from a culture of prevention to one of after-the-fact treatment and vaccines. But if the severity of the COVID-19 pandemic has taught us anything, it is that the wait for a vaccine can be excruciating — not to mention economically devastating.
There also have been a limited number of cases when, applied or used improperly, temporary injuries have occurred. However, given proper application and basic safety measures, UVGI is quite safe and is not associated with any long-term health effects. Education is key for this technology to assume its rightful place in healthy building strategy and pandemic preparedness. That begins with a brief explanation of UV irradiation and how it can be manipulated to inactivate disease causing microbes.
What Is UVGI and How Does It Work?
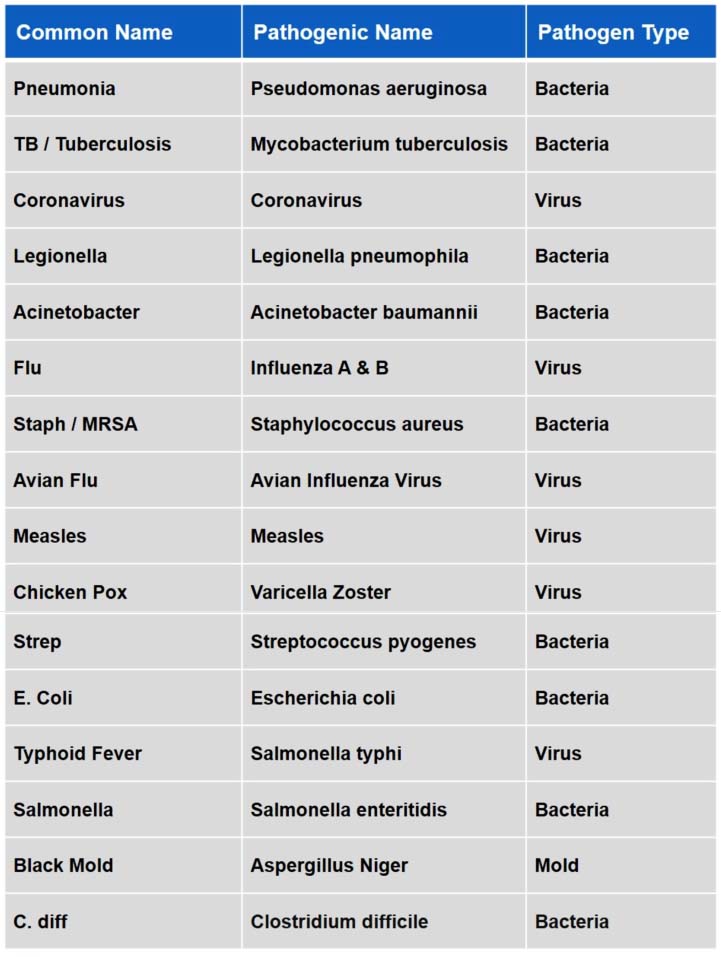
UV light, an electromagnetic radiation, is classified into four wavelength ranges, referred to in nanometers (nm): vacuum UV (100 to 200 nm), UV-C (200 to 280 nm), UV-B (280 to 315 nm), and UV-A (315 to 400 nm). Of these, UV-C light is most useful as a means of disinfection. At this particular range UV light is absorbed by the DNA, RNA, and proteins of biological organisms. When this absorption occurs, the organism is no longer able to replicate or infect other organisms, including people. The duration and level of UV-C exposure required for deactivation varies slightly from microbe to microbe, but generally deactivation is within seconds. (See Table 1 for a listing of well-known pathogens that have been deactivated by UV-C light as of the writing of this article.)
Table 1: Well-Known Pathogens Deactivated Through UVC
Click table to enlarge
In UVGI applications, UV-C at wavelengths close to 254 nm is delivered through low- pressure mercury vapor lamps that can be applied in several ways to disinfect air, surfaces, and even drinking water.
UV-C lamps for surface applications can either be fixed or portable and are intended for use in spaces that are presently unoccupied. UV-C lamps for air disinfection are typically applied in one of two ways: They can be installed within the mechanical air handling system of a building (a method known as “in-duct” UVGI) to disinfect building supply air; or they can be included as part of specially designed fixtures that are installed on walls and/or ceilings to disinfect the air within a space. The latter method, commonly referred to as “upper air” or “upper-room” UVGI, specifically targets contaminants within an occupied space, while in-duct UV-C treats supply or recirculated air prior to its delivery to the space. As such, upper-room UVGI treats air close to the contaminant source (people), making it particularly effective at preventing person-to-person spread.
Upper-room UVGI fixtures can be either wall-mounted, suspended from the ceiling, or both, depending on the size and geometry of the room. The fixtures may be open or louvered depending on the ceiling height. Louvered fixtures can be safely installed in rooms that are eight to nine feet high as long as the bottom of the fixture is at least 7 feet from the floor. The louvers direct and confine the irradiation from the UV-C lamps to the germicidal field, which is usually no greater than six inches from the ceiling. Open or non-louvered fixtures direct germicidal energy into the entire upper-room area and can be safely used in rooms with ceilings that are over nine feet high.
Air movement (created by the natural rise and fall of convection, existing HVAC, or in some cases paddle fans) helps to “herd” exhaled viruses and other room contaminants into the irradiation zone. Eradication is fast, typically within seconds depending on the dose of UV-C irradiance energy and the particular virus or bacteria.
Visual Sense of Security
What makes upper-room UVGI particularly appealing in the age of COVID-19 is that it can be easily and affordably applied to existing buildings. Unlike in-duct systems, it doesn’t require HVAC expertise to apply or install. Some applications may require hidden wiring, in which case an electrician may be needed, but in many cases the lights can be installed by properly trained facility maintenance personnel. UVGI manufacturers and their representing agents can access the particular application and help select appropriate equipment.
According to Mike Shea, president of the Tom Barrow Company, it is the literal and psychological accessibility of upper-room UVGI that makes it especially relevant given the hardships of the COVID-19 pandemic. Shea has supplied UV-C products along with the many airside HVAC products that his company has sold for many years. However, it wasn’t until the recent pandemic that he was confronted with such a high demand specifically for upper-room UVGI.
“Upper-room is much easier for the average business owner to understand. For one thing, it isn’t hidden away in the mechanical system. People can see it working. And right now people really want that visual sense of security when they enter into a space,” said Shea.
Since the start of the pandemic, Shea has sold upper-room UVGI fixtures for dentist offices, gyms, K-12 classrooms, universities, offices spaces, churches, and more. The demand was there even before scientists had had a chance to test the effects of UV-C on the new virus. Since then, evidence has been mounting that UV-C is effective against SARS-CoV-2.
Ultraviolet Light Vs. SARS-CoV-2
Long before COVID-19, a wealth of evidence had proven UV-C light as an effective intervention against the transmission of airborne diseases. More recently, the scientific community has published work that validates UV-C light as specifically effective against SARS-CoV-2.
In October 2020, the American Journal of Infection Control published a report, Susceptibility of Sars-CoV-2 to UV Irradiation, asserting the following:
- SARS-CoV-2 is highly susceptible to irradiation with ultraviolet light.
- High viral loads of 5 x 106 TCID50/ml SARS-CoV-2 can be inactivated in nine minutes by UVC irradiation.
- UVC irradiation represents a suitable disinfection method for SARS-CoV-2.
Data from the study “confirm former findings that UV-C is more effective in inactivating viruses and highlight UVC irradiation as an effective method for the inactivation of SARS-CoV-2.”
Results from another study conducted and drafted by scientists at Boston University show that “UV-C is a powerful tool that can be applied extensively in a wide range of public institutions including hospitals, nursing homes, workplaces, schools, airports, and shopping centers to disinfect contaminated equipment and surfaces to prevent and reduce SARS-CoV-2 contact transmission.” As of this writing a preliminary report from the study has been published online and awaits peer review.
Regarding upper-room UVGI specifically, results from a peer-reviewed feasibility study “strongly suggest that upper-room UVGI, if applied correctly, should be effective at disinfecting SARS-CoV-2 virions suspended in respiratory droplets in the air.”
Application and Education Is Key to Safety
Safety remains a concern in the minds of many, largely because many fail to recognize that neither in-duct nor upper-room UVGI equipment is designed or intended for direct exposure to human skin. However, as long as equipment is properly installed and safety protocols observed, upper-room UVGI can be safely installed in a variety of spaces.
Unlike solar UV exposures, UV-C radiation does not penetrate beyond the “dead” outer layer of the skin and therefore is not associated with the same long-term effects. That said, direct exposure of the skin or eyes to UV-C radiation can cause erythema (“sunburn”} and photokeratitis (“welder’s flash”) to the eyes. Even though upper-room UVGI may be operating while a room is occupied, that does not mean occupants are being directly exposed because non-reflective louvers channel radiation within a narrow field, well above the heads of occupants. Students in a classroom can lie flat on their backs and stare at the ceiling without incurring any harm. Direct exposure would be akin to someone climbing on a ladder and putting themselves within the irradiation field. Otherwise normal room movement and occupation presents no danger.
What accidents have occurred have been attributed to improper installation and human error. This has been the conclusion of at least one double-blind, placebo-controlled field trial of upper-room UVGI at 14 homeless shelters in six U.S. cities from 1997 to 2004. The study concluded:
- “Upper-room UVGI has the potential to offer significant protection at relatively low cost and is especially well-suited for retrofitting older buildings. Based on the results reported here, concerns regarding safety — particularly the possibility of photokeratitis conjunctivitis and skin erythema from excessive UV-C exposure — should not deter application of carefully designed and maintained upper-room UVGI systems.
- [….] current upper-room UVGI technologies, with proper engineering, installation, and maintenance, can be placed safely in a wide range of indoor spaces, even in buildings as diverse as homeless shelters. [ …] With a greater understanding of the application of UVGI, the full potential of this technology to improve control of person-to-person transmission of human airborne pathogens in buildings should be realized.”
In addition to proper installation and maintenance, there are certain precautions and protocols that should be observed. These include, but may not be limited to, worker training, the posting of signage that informs occupants about the presence of the UVGI devices, safe maintenance procedural training, and in some cases the installation of sensors to detect any movement within the radiation field and associated alarms or shut-offs. The FDA also suggests (and the author of this article concurs) that anyone considering implementing the technology should ask the following questions of UV-C equipment manufacturers:
- What health or safety risks are associated with the equipment?
- What instructions for use or training are available or provided for the product?
- Does product generate ozone? (Note: Ozone is only produced at wavelengths lower than 200nm, therefore germicidal UVGI lamps at 254 nm should be ozone free.)
- How should broken or damaged lamps be handled and disposed?
To ensure uninterrupted service in the future, prospective buyers should also inquire about the availability of replacement lamps. Some manufacturers use proprietary lamps in their fixtures which can be very expensive and difficult to find, especially during high-demand periods. Non-proprietary lamps are generally widely available, much less expensive, and can even be ordered online.
Making Old Air New Again
Throughout the pandemic, we’ve all been coached on the value of ventilation, filtration, and dilution as a way to purge indoor air of disease-causing pathogens, but these are not stand-alone strategies.
For example, to mitigate the risks of COVID-19, ASHRAE now recommends upgrading HVAC air filters to MERV-13 or higher if possible.
ASHRAE also recommends increasing ventilation and operating systems with 100% outdoor air whenever possible. Unfortunately, many buildings are designed to recirculate a certain amount of pre-conditioned, return air. They do not have the capacity to fully condition (heat, cool, humidify and dehumidify) every bit of indoor supply air. And even if they do, this is highly cost-prohibitive to most owners.
“We’ve seen this a lot in the past year. One university decided to operate all their buildings at 100% outdoor air even though it was not designed to operate that way. It was done knowing that it could create many other problems, like mold,” said Shea.
The application of upper-room UVGI can, to a degree, make old air fresh again by inactivating biological contaminants like mold, bacteria, germs, and viruses. This has been demonstrated in various studies using a commonly used metric for ventilation, air changes per hour (ACH).
ACH, quite simply, refers to how often the air in a space is completely replaced. The higher the ACH, the lower the risk of spreading airborne disease. For example, current CDC guidelines for health-care facilities require a minimum of six air changes for all rooms. Some spaces, like operating rooms, require 15 or more ACH. An ACH of four is the minimum recommended air change rate for most commercial buildings. Often, studies that measure the efficacy of UVGI to inactivate specific airborne pathogens are compared to the number of ACH that would be needed to eliminate the same pathogens using normal ventilation.
Upper-room UVGI is not only less expensive than physically creating air changes using mechanical ventilation, but also more effective. In a study published in 2002, researchers at the Harvard School of Public Health found that when it came to reducing the concentration of two common bacterium, one causing tuberculosis and the other associated with a number of hospital-acquired infections, upper-room UVGI produced equivalent ventilation ranging from 6.4 ACH to 28.5 ACH using ceiling and wall-mounted [UVGI] fixtures.
Another study, which focused on the virus that causes smallpox, yielded even more impressive data with regard to equivalent air changes using upper-room UVGI.
“Using vaccinia virus aerosols as a surrogate for smallpox we report on the effectiveness of air disinfection, via upper-room UVC light, under simulated real world conditions including the effects of convection, mechanical mixing, temperature and relative humidity. In decay experiments, upper-room UVC fixtures used with mixing by a conventional ceiling fan produced decreases in airborne virus concentrations that would require additional ventilation of more than 87 air changes per hour. Under steady state conditions the effective air changes per hour associated with upper-room UVC ranged from 18 to 1000.”
But what about SARS-CoV-2? Can similarly high ACH rates be attained using upper-room UVGI to remove the virus that causes COVID-19? Per the same peer reviewed feasibility study referenced earlier in this paper, it is expected that it can:
“Through analysis of expected and worst-case scenarios, the efficacy of the upper-room UV-C approach for reducing COVID-19 transmission in confined spaces (with moderate but sufficient ceiling height) is demonstrated. Furthermore, it is shown that with SARS-CoV-2, it should be possible to achieve high equivalent air change rates using upper-room UV air disinfection, suggesting that the technology might be particularly applicable to poorly ventilated spaces.”
Although direct evidence is lacking due to the novelty of the COVID-19 virus, Table 2 summarizes the equivalent ACH rates for reduction of airborne contaminants.
Table 2
Click table to enlarge
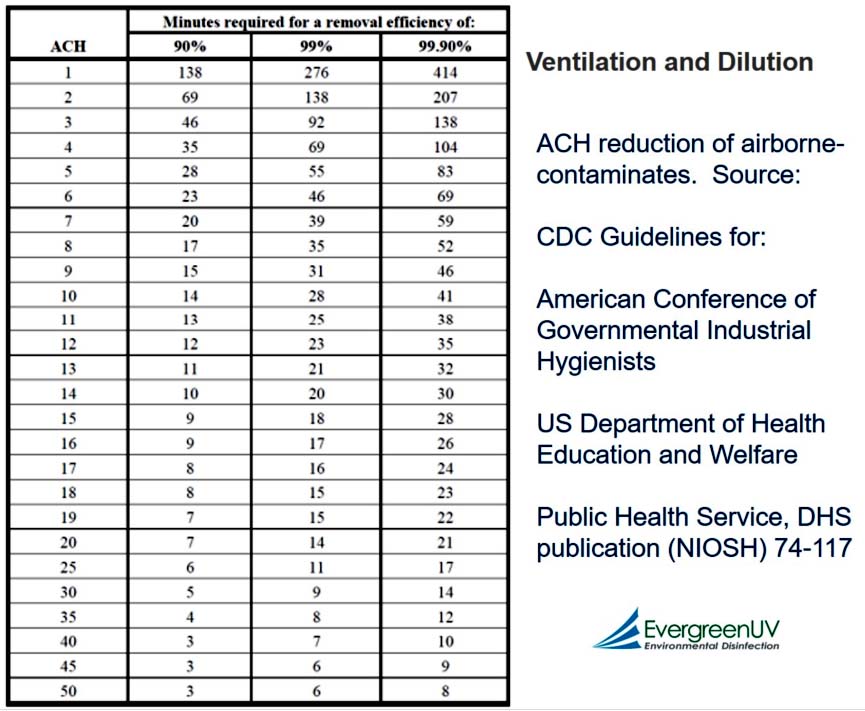
“There is no overstating the significance of this to building owners. Upper-room UVGI provides a level of airborne germicidal treatment that, practically and affordably speaking, neither filtration nor ventilation can. And it’s accessible – both to sprawling universities as well as bars and restaurants,” said Shea.
Shea also added that without some sort of supplementary strategy like UVGI, building owners that seek to meet the latest ASHRAE 90.1 energy guidelines ultimately will be spinning their wheels while also trying to mitigate the spread of COVID-19 with filtration and ventilation alone. Even ASHRAE in its 2020 Position Document on Infectious Aerosols, acknowledges that the design and operation of HVAC systems are only “one part of an infection control bundle” while calling out UVGI as a “well researched and validated” strategy.
Conclusion
As the world waits for widespread immunity to the COVID-19 virus, each of us is confronted with the same two questions almost daily: What can we do to stay safe (and solvent) in the meantime? And what can we do to lessen the impact of future infectious outbreaks? Upper-room UVGI is a potential antidote to the helplessness that many feel, particularly business owners and institutions whose activity and livelihoods have been upended in the last year. The solution is easily retrofitted and a visual reminder to building occupants that the air within a given space is continuously being cleaned of harmful pathogens. The technology is well researched with a long track record of success against some of the most contagious diseases known to man. It has earned the rights to a prominent position in fight against COVID-19, as well as a preparedness strategy for future health crises.


Report Abusive Comment