The following is excerpted from ASHRAE’s “Alternate Care Site HVAC Guidebook.” SNIPS is including it here with the hopes that all contractors will be able to utilize its information in the building of alternate care sites.
The Coronavirus pandemic created unprecedented challenges to the nation’s healthcare system. USACE was tasked with the design and construction of Alternate Care Sites (ACS) to relieve the strain on the health care system. The ASHRAE Alternate Care Sites Task Force was convened upon the request to the ASHRAE Epidemic Task Force from the USACE Headquarters to provide engineering recommendations, solutions, and guidance to address the HVAC systems for ACS.
ACS are temporary facilities that are used as flexible patient care space to limit the overload of hospitals and other urgent care facilities during the pandemic to allow them to treat the most severely ill patients.
Alternate Care Site HVAC Guide Book Objectives
Coronavirus Disease 2019 (COVID-19) is a respiratory tract infection caused by a newly emergent coronavirus, SARS-CoV-2, that was first recognized in Wuhan, China, in December 2019. Genetic sequencing of the virus suggests that SARS-CoV-2 is a beta coronavirus closely linked to the SARS virus.
While most people with COVID-19 develop mild or uncomplicated illness, a percentage develop severe illness requiring hospitalization and oxygen support, and some requiring admission to an intensive care unit and use of ventilators. In such severe cases, COVID-19 can be complicated by Acute Respiratory Disease Syndrome (ARDS), sepsis, and septic shock, multi-organ failure, including acute kidney failure as well as cardiac injury. Older age people with comorbid diseases appear to have greater risk factors for death due to additional complications.
This guide is being developed in response to a need for ACS to be deployed in locations where permanent hospital beds are insufficient for the number of COVID-19 positive patients needing care. The guidance included in the later sections is meant to apply specifically to COVID-19 patient care but would be generally applicable to similar viruses transmitted as airborne infectious aerosols and through droplets. Project teams for future ACS deployment would need to review the requirements shown in this guidebook to determine which may be applicable to epidemics or pandemics for similar viruses.
Scope of the Guide
This guide will primarily be applicable to host sites with large open spaces as outlined in the table below. Most of the recommendations are suitable for Arena to Healthcare (A2HC) situations. Convention Centers and other “large spaces” are included in guidance for A2HC. Conversion of smaller large space facilities such as school gymnasiums would also be applicable to a high degree. These are several of the most robust types of ACS which may operate throughout the year while offering greater flexibility in approach to the design and construction of the overall ACS. Closed Hospital to Health Care (CH2HC) will also be applicable. Many of the requirements from ASHRAE Standard 170 and other references will be directly applicable to the CH2HC sites.
Hotel, dormitory, barracks, and tent ACS facilities will have the least applicability to this guide. Hotel sites are limited in the retrofit that may take place to return the facility back to hotel usage when the ACS is no longer required. Tent locations, due to the inability to maintain a tight envelope, are only suitable during temperate weather conditions which may limit their use depending on the local climate.
Based on these limitations the hotel, dormitory, barracks, and tent facilities may not holistically use this design guide although some of the reference material and principles contained in its sections may be useful.
Contaminant Control
Contaminant control through dilution by ventilation in buildings has been a topic of interest in the HVAC industry since 1973 when ANSI/ASHRAE Standard 62 was first published. In 1986, the World Health Organization reported a significant number of newly constructed western buildings were not properly ventilated, leading to the phrase “sick building syndrome” to be coined and used hence forth as a catalyst to increase awareness and drive change within commercial building ventilation requirements. In 2004, ASHRAE Standard 62 was split into commercial and residential sections (62.1 & 62.2) and is now the common building standard for ventilation requirements. Then, in 2008, ASHRAE Standard 170 was published to provide ventilation guidance that is specific for healthcare facilities. In conjunction with these standards and others related to the human environment and what we know about the mitigation of viral dispersion, the following approaches are minimum design requirements and optimal practices for temporary facilities used as wards for infected patients. The use of any facility for non-infected patients, as a spill-over facility, should utilize the existing system approach if it can meet or exceed the minimum requirements necessary for proper patient care.
This guidebook aims to provide recommendations in applying these standards which are used for permanent facilities to temporary sites under less than ideal conditions or with time, budget, and technical feasibility constraints.
Airflow Approaches and Methods of Supply and Exhaust
Contaminant capture and removal effectiveness depends greatly upon supply and exhaust strategies. These strategies depend on the type of facility in which they are employed, and this document addresses the following two major categories, large open spaces such as arenas or convention space, and typical hotel style rooms. The versatility and availability of arenas and convention centers make them prime locations for alternate care sites. Large spaces should be targeted for acute and non-acute care patients. Confined spaces like hotels, barracks and dorms are more appropriate for non-acute care.
Supply systems used for treating airborne infectious disease should be designed as all outdoor air systems to avoid cross-contamination of air from different zones. Existing return ducts should be disconnected, and new ductwork sealed to allow the system to operate with 100% outside air. If the coil capacity of the existing system is not able maintain temperature and humidity in 100% outside air mode, a return air mode may be utilized if the return air ductwork is retrofitted to include a MERV 8 pre-filter and a HEPA filter complemented by a booster fan if needed to overcome additional pressure drop of the filter banks. This option will require additional time and resources and it may be more cost effective to discharge return air cleaned by a HEPA filter unit directly to the ACS interior space. Supply systems for fully enclosed pods do not require 100% outside air if the patient pod air is exhausted directly outside per Standard 170 requirements or HEPA filtered before being discharged to the ACS interior space. These scenarios allow designers to determine how they can provide the minimum required air changes to the patient spaces safely, effectively, and efficiently as possible.
All areas with potential viral loading, such as doffing areas, rooms with used PPE, or common areas that patients could access during their time at the facility, would be subject to the HEPA filtered exhaust requirement if exhaust air is not purged directly outside per ASHRAE Standard 170 requirements. Restrooms are also to be exhausted to the outside.
Supply Air System Selection air system selection. Prioritization of system approach in order of preference:
- Supply systems use 100% OA, all potentially viral loaded air is exhausted outside per ASHRAE Standard 170 requirements.
- Supply systems uses return air from ACS interior spaces:
- Potentially viral loaded air is exhausted outside per ASHRAE Standard 170, return air is only from clean spaces in the facility (unused exhibit halls, admin areas, corridors, etc.)
- Potentially viral loaded air is exhausted through HEPA filters and returned to ACS interior
- Supply systems use return air from ACS interior spaces, if potentially viral loaded air is in the general return, the AHU would have HEPA filters on the mixed air section. The increased pressure drop can be overcome by increasing the filter surface area, upgrading AHU fan size, or introducing booster fans. This would be most applicable to the open patient bed scenario where the viral loaded arena air does not utilize ducted exhaust.
Based on the desired system approach, to achieve the required minimum airflow requirements and maintain comfort conditions within the arena and patient spaces, there are three supply air delivery approaches that should be considered:
1. Existing AHU has the capacity/functionality to meet the minimum requirements (Figure 3-1).
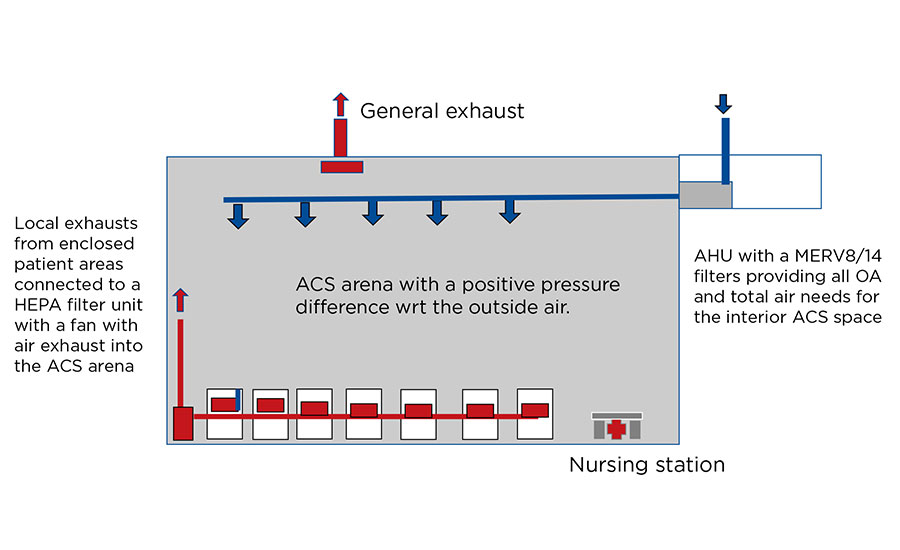
Photo by: yienkeat/iStock/Getty Images Plus via Getty Images
The figure above is an example of ventilation and conditioning of enclosed patient spaces located in the building without perimeter zone using existing DOAS AHU, air distribution, and general exhaust systems. AHU is upgraded with MERV 8 prefilters and MERV 14 final filters providing all outside air needs (including for enclosed patient areas, nursing stations, etc.) and a positive pressure difference in ACS with respect to outside. ACS air is forced into enclosed patient space via transfer grill under the negative pressure created by a headboard exhaust. A HEPA filter box with a fan is connected to a group of headboard exhausts. Cleaned air is discharged back into the upper zone of ACS.
2. Combination of existing AHU and temporary AHU to achieve minimum requirements (Figure 3-2).
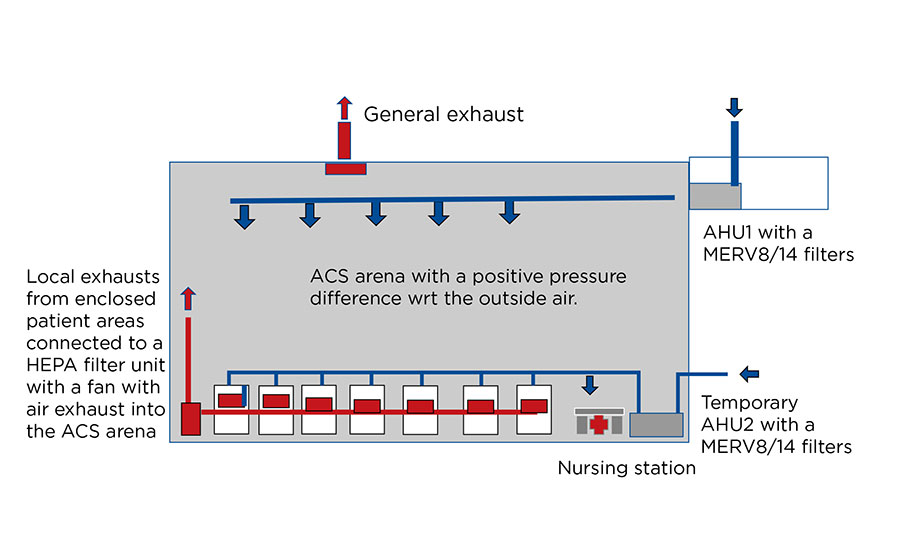
Photo by: yienkeat/iStock/Getty Images Plus via Getty Images
The figure above is an example of ventilation and conditioning of enclosed patient spaces located in the building without perimeter zone using existing DOAS AHU, air distribution and general exhaust systems. AHU is upgraded with MERV 8 prefilters and MERV 14 final filters and the airflow rate is adjusted to provide outside air needs of all ACS areas except for enclosed patient areas, and a positive pressure difference in ACS with respect to outside. Clean and conditioned outside air is supplied into enclosed patient space from the temporary AHU equipped with a MERV 8 prefilters and MERV 14 final filters and is exhausted using headboard exhaust at a higher rate to created negative pressure in the patient space with respect to the ACS space. A HEPA filter box with a fan is connected to a group of headboard exhausts. Cleaned air is discharged back into the upper zone of ACS
3. Temporary AHU used in place of existing with capacity/functionality to meet minimum requirements (Figure 3-3).

Photo by: yienkeat/iStock/Getty Images Plus via Getty Images
The figure above is an example of ventilation and conditioning of enclosed patient spaces located in the building without perimeter zone using temporary DOAS AHU, new air distribution and existing general exhaust systems. Existing AHU and air distribution system are abandoned. Clean and conditioned outside air is supplied into all ACS spaces and into enclosed patient spaces from the temporary AHU2 equipped with a MERV 8 prefilter and MERV 14 final filter and is exhausted using headboard exhaust at a higher rate to created negative pressure in the patient space with respect to the ACS space. A HEPA filter box with a fan is connected to a group of headboard exhausts. Cleaned air is discharged back into the upper zone of ACS. Existing general exhaust is adjusted to maintain positive pressure in ACS with respect to the outside air.
This article originally appeared in the January 2021 issue of SNIPS Magazine.



Report Abusive Comment